Chronic kidney disease (CKD) is the ninth leading cause of death worldwide, with rates increasing in recent years. While its causes may vary from country to country, it consistently affects 8-12% of the population, regardless of region or national income level. Once the kidneys fail, only dialysis or kidney transplantation can save that person’s life.
Dialysis is a life-sustaining medical treatment that filters waste products and excess fluid from your blood when your kidneys fail, essentially acting as an artificial kidney. While it can save lives in the short term, it requires three, four-hour treatment sessions weekly for the rest of a person’s life and comes with a multitude of medical complications.
Ultimately, fewer than 65% of people on dialysis in the U.S. live longer than five years (a number that is even lower in low-resource settings). By contrast, kidney transplantation, while itself a complex process, can liberate a person from the need for dialysis, resulting in a five-year survival rate greater than 80%.
University of California, San Francisco (UCSF) surgical resident and lead researcher Alan Zambeli-Ljepović, MD, MHS, says “it’s a no-brainer” that we should do our best to transplant every patient who would stand to benefit from the operation. “But it’s not the trend we’re seeing around the world.” While access to dialysis has been increasing globally, fewer people have access to kidney transplantation today compared to five years ago.
Zambeli-Ljepović and colleagues wanted to estimate how many lives could be saved if some of the investments in dialysis infrastructure were shifted toward kidney transplantation.
How They Did It
For the study, researchers looked at countries that offer both treatments for kidney failure and collected data on global disease prevalence, population and finances, and dialysis and kidney transplantation rates. Sources included the World Bank, the Institute for Health Metrics and Evaluation, the Global Observatory on Donation and Transplantation, the International Society of Nephrology–Global Kidney Health Atlas, and more.
Collecting data was no small feat, but the real challenge was using it in an unbiased and effective way. For example, there is significant variation in how kidney disease is diagnosed across countries, making it difficult to assess how effectively it is being treated. To account for some of these differences, the team used a novel metric in the field of kidney disease (mortality-to-prevalence ratio) and adjusted for other factors, including GDP per capita and national age distribution. Then they assessed the relationship between current rates of dialysis and transplantation and mortality from kidney disease across 203 countries. They found that simulating the effect of a subtle shift in investment (on a national level) from dialysis to transplantation would save at least 290,000 lives annually.
A Collaborative Approach
A study of this depth requires skills beyond surgery, including a thoughtful approach, statistical modeling, and gathering input from experts across world regions and medical and scientific specialties. The authors of this research, published in The Lancet, came together as part of the African Transplant Research and Sustainable Development Group, which meets monthly to advance research and other projects focused on capacity building for countries with young transplant programs.
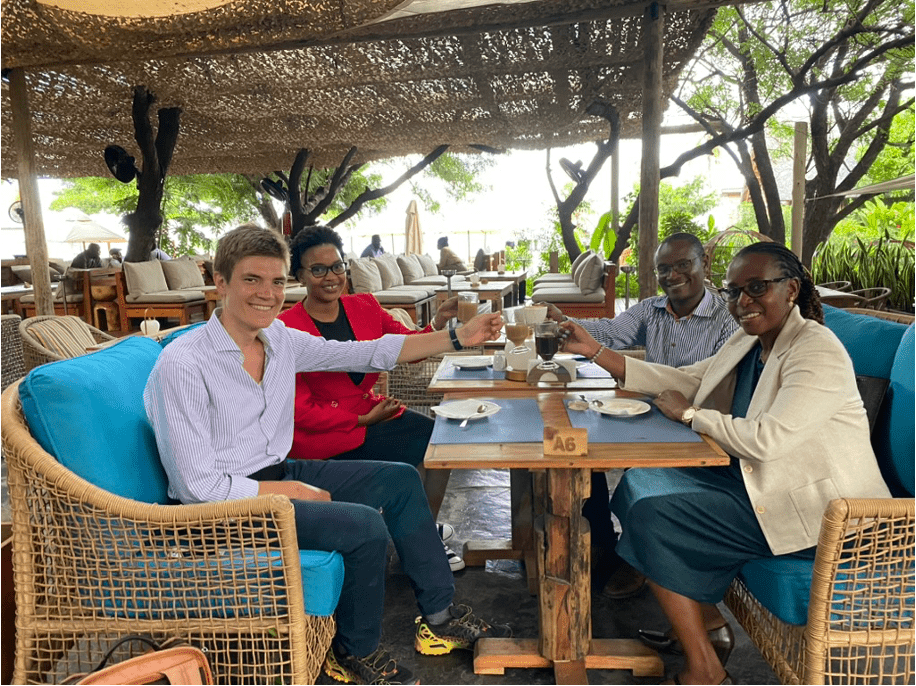
This group was started by Zambeli-Ljepović, who is also a fellow of the Center for Health Equity in Surgery and Anesthesia (CHESA) at UCSF’s Institute for Global Health Sciences. He has devoted mentors who believed in the project, despite working across different divisions within the Department of Surgery. John Rose, MD, MPH, a reconstructive plastic surgeon and senior author of the Lancet paper, emphasized the role of CHESA at UCSF. “This research required an incredible amount of collaboration and coordination,” he says. “CHESA facilitated this collaboration by creating a network of researchers from around the world.”
Many of the researchers involved, including co-authors Fransia Arda Mushi, MD, and Mekdim Tadesse Siyoum, MD, were Zambeli-Ljepović’s co-fellows in CHESA. Peter Stock, MD, a UCSF transplant surgeon who led the effort to enable transplantation among HIV-positive patients (signed into federal law as part of the HOPE Act of 2012), played a major role as one of Zambeli-Ljepović’s mentors who helped build this group. Other collaborators include Nancy Ascher, MD, PhD, a globally recognized transplant surgeon and staunch advocate for equitable access to transplantation, and Stefano Bertozzi, MD, MPH, a UC Berkeley professor of public health and leading clinical advisor behind the Gates Foundation’s push to make antimicrobials more affordable around the world.
Additional Policy Questions
Despite the compelling findings, Zambeli-Ljepović says the decision to choose transplantation over dialysis “is nuanced,” for both the individual and at the policy level. Transplantation relies on complex medical infrastructure that is susceptible to unstable government financing, conflict, and inconsistent access to essential medications and testing. The team is now working with their international colleagues to tackle these hurdles.
Next, they want to determine how to decide whether to invest in transplantation or dialysis with a limited budget. UCSF health economist Tracy Lin, PhD, is helping assess the value proposition of transplantation versus dialysis in Tanzania to create a model applicable to any setting. The team is also working with Bertozzi and international partners to identify strategies to mitigate the exorbitant costs of transplant-related medications, which appear to be a key limiting factor in low-income settings.
Alongside his primary career goals as an abdominal transplant surgeon, Zambeli-Ljepović plans to continue his research. “As an expert transplant surgeon who understands how transplant systems are built,” he says, “I can play a bigger role in developing self-sustaining transplant programs around the world.” When it comes to global health, he says, “We have much to give and much to learn from others.”
Read the study: The potential of kidney transplantation to reduce mortality from chronic kidney disease: a global, cross-sectional, modelling study

